

Treatment with antiviral agents may lessen the risk of disease in the fellow eye, but variations in treatment regimens to include intravenous, oral, or intravitreal medication do not seem to influence the frequency of retinal detachment.
Proof that herpetic viral infection causes this syndrome led to the use of specific antiviral therapies to halt progression however, late retinal detachment remains a serious complication that may limit recovery of vision. Visual prognosis is guarded, especially after retinal detachment. Treatment is directed toward rapid control of infection and infection as well as surgical management of complications such as retinal detachment. Diagnostic testing often includes syphilis serology, as well as PCR amplification eye fluid for herpes simplex, varicella, cytomegalovirus, and occasionally Epstein-Barr virus and toxoplasma. Optic neuropathy or atrophy, scleritis, and pain occur in some patients but are not part of the AUS diagnostic criteria.

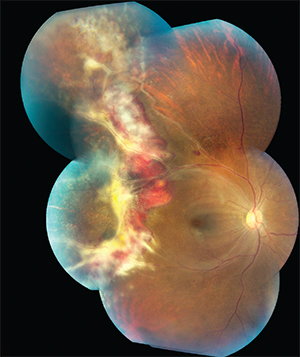
(AUS) is that the term acute retinal necrosis be applied only to those cases that conform to the clinical syndrome characterized by peripheral retinal necrosis with discrete borders, rapid progression with circumferential spread in untreated eyes, occlusive vasculopathy with arteriolar involvement, and prominent inflammation in the vitreous and anterior chamber. Consensus among members of the American Uveitis Society The syndrome is now recognized to be predominantly the consequence of acute infection of the retina by alpha class Herpesvirus hominis. Initially described in Japan in 1971 by Urayama and colleagues and termed Kirisawa’s uveitis, acute retinal necrosis (ARN) is a sudden onset unilateral or bilateral panuveitis that presents with iritis, vitreous inflammation, retinal periarteritis, optic neuropathy, and confluent peripheral retinal infiltrates. Varicella-zoster necrotizing retinopathy.Herpes simplex 2 necrotizing retinopathy.Herpes simplex 1 necrotizing retinopathy.Consensus among members of the American Uveitis Society is that the term acute retinal necrosis be applied only to those cases that conform to the clinical syndrome characterized by peripheral retinal necrosis with discrete borders, rapid progression with circumferential spread in untreated eyes, occlusive vasculopathy with arteriolar involvement, and prominent inflammation in the vitreous and anterior chamber.


 0 kommentar(er)
0 kommentar(er)
